How sleep quality influences GI symptoms and emotional well-being in children
Written by Anna Katherine Black, PhD
Licensed Clinical Psychologist
GI Psychology
If your child struggles with stomach problems—like nausea, bloating, or pain—you’ve probably noticed that sleep plays a big role. Poor sleep or insomnia can worsen not just gut symptoms but also mood, anxiety, and overall emotional well-being. Scientists call this the gut-brain axis—the constant, two-way communication between the brain and the gut. And for kids with gastrointestinal (GI) conditions, this connection is especially powerful.
Understanding how sleep quality affects both the brain and the gut can help parents, caregivers, and clinicians support children more effectively.

Why Sleep Matters for Children with GI Issues
Sleep is not just “rest.” During sleep, the brain processes emotions, repairs the body, and regulates hormones that influence digestion and immune function.. When children don’t get enough quality sleep:
- Their GI symptoms—such as abdominal pain, diarrhea, or constipation—can worsen (Barberio et al., 2021).
- Their emotional resilience drops, making it harder to cope with stress, flares, or medical procedures (Crohn’s & Colitis Foundation, 2023).
- Their risk of developing anxiety or depression increases, both of which can further disrupt the gut-brain axis (American Psychological Association [APA], 2022).
In fact, research suggests that 30–60% of children and adolescents with inflammatory bowel disease (IBD) or functional GI disorders report significant sleep disturbances (Palsson et al., 2024; Rome Foundation, 2024).
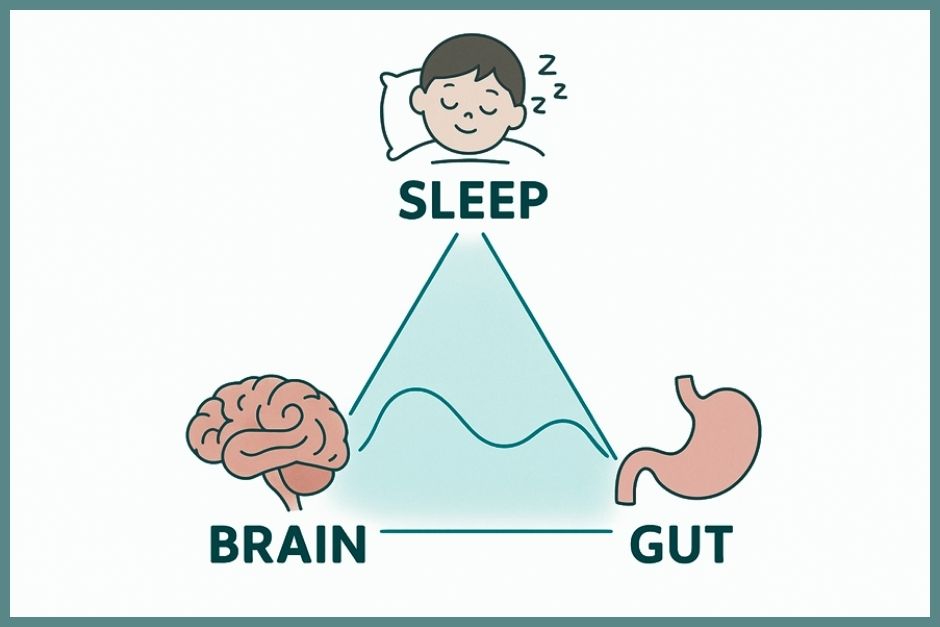
The Gut-Brain-Sleep Triangle
Think of sleep, the brain, and the gut as three points of a triangle. If one side is disrupted, the others wobble too:
- Insomnia → leads to higher inflammation in the gut and more pain sensitivity (Keefer & Keshavarzian, 2006).
- Gut symptoms → like cramping or nausea, keep kids awake at night (Barberio et al., 2021).
Emotional distress → anxiety about flares or procedures can trigger both insomnia and GI upset (Chen et al., 2021).
This cycle has been confirmed in both adults and children: one randomized controlled trial found that cognitive-behavioral therapy for insomnia (CBT-I) improved both sleep quality and GI symptom severity in youth with functional abdominal pain (Palsson et al., 2024).
Supporting Kids: Practical Tips for Parents
Parents often ask, “What can we actually do?” Here are some supportive steps backed by sleep medicine and GI psychology:
- Create a calming bedtime routine: Gentle breathing, reading, or listening to relaxation recordings can help the brain “switch off.”
- Keep sleep and wake times consistent—even on weekends. This trains the body’s clock.
- Limit late-night screen use: Blue light delays melatonin, the hormone that helps kids fall asleep.
- Talk openly about worries: A brief check-in before bedtime can prevent anxiety from showing up at 2 a.m.
- Explore gut-brain therapies: GI-focused CBT, clinical hypnosis, and mindfulness have all been shown to reduce symptom-related insomnia in children (Chen et al., 2021; Keefer & Keshavarzian, 2006).
Conclusion: Building Health Through Rest
For kids with stomach problems, sleep is not a luxury—it’s a powerful part of healing. Supporting quality rest can ease symptoms, improve emotional well-being, and strengthen the gut-brain axis.
If your child is struggling, know that help is available. Licensed clinicians trained in GI psychology and behavioral sleep medicine can provide tools that go beyond medication, helping your child feel better day and night.
- Printable resources and educational support
- Schedule a consultation with our team to see how GI Psychology can support your child and family
- Reach out directly: admin@gipsychology.com
References
American Psychological Association. (2022). Managing stress and gut health. American Psychological Association. https://www.apa.org
Barberio, B., Zamani, M., Black, C. J., Savarino, E. V., Ford, A. C., & Storr, M. A. (2021). Prevalence of anxiety and depression in inflammatory bowel disease: Systematic review and meta-analysis. Alimentary Pharmacology & Therapeutics, 54(8), 952–961. https://doi.org/10.1111/apt.16563
Chen, E., Sweeney, C., Keefer, L., & Szigethy, E. (2021). Cognitive behavioral therapy for youth with inflammatory bowel disease: Effects on sleep and symptom management. Journal of Pediatric Psychology, 46(9), 1051–1062. https://doi.org/10.1093/jpepsy/jsab050
Crohn’s & Colitis Foundation. (2023). Sleep and IBD: Why it matters. Crohn’s & Colitis Foundation. https://www.crohnscolitisfoundation.org
Keefer, L., & Keshavarzian, A. (2006). Feasibility and acceptability of gut-directed hypnotherapy for patients with inflammatory bowel disease: A brief report. Alimentary Pharmacology & Therapeutics, 24(5), 759–766. https://doi.org/10.1111/j.1365-2036.2006.03036.x
National Institutes of Health. (2021). Why sleep is important. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health/sleep/why-sleep-important
Palsson, O. S., van Tilburg, M. A., & Whitehead, W. E. (2024). Behavioral sleep interventions for youth with functional abdominal pain: A randomized controlled trial. Neurogastroenterology & Motility, 36(3), e14562. https://doi.org/10.1111/nmo.14562
Rome Foundation. (2024). Disorders of gut-brain interaction (DGBI). Rome Foundation. https://theromefoundation.org
